Chest osteochondrosis (GO) of the spine is rarely diagnosed, in contrast to cervical and lumbar osteochondrosis, which occurs in 2-3 patients over 18 years of age. This phenomenon is explained by the special structure of the chest - the presence of a larger number of plates, which in turn have a finer structure. This part of the spine is of low mobility and, accordingly, the load is not great, since the main "blow" is taken up by the sternum together with the ribs.
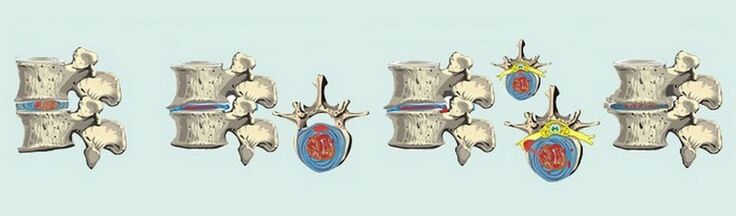
The main cause of chest pathology is an increase in the load on the intervertebral discs and, as a result, a violation of metabolic processes and their structure.. . . In the case of such a disease, the shock-absorbing properties of the disc are lost, the fibrous ring becomes thinner, dries out, then the nerve endings become inflamed, the person feels constant pain and discomfort, and motor activity decreases. . With the rapid course of the disease, it affects the ligaments of the spine and joints.
Now, many experts have adopted the rule that osteochondrosis is not classified according to the stages of the course, but according to its degrees, which are also distinguished by the characteristics of the symptoms.
Considering the general symptoms, osteochondrosis of the thoracic region is less pronounced, in contrast to other types, yet there is a characteristic clinical picture. Thus, the patient may complain of the presence of the following signs:
- pain in the chest region, often exacerbated by prolonged exposure in one position or at night;
- painful sensation between the shoulder blades while increasing with arm lifting or after physical exertion;
- discomfort, pain during deep breathing, this symptom can also be observed on exhalation;
- while walking the ribs are sore and a tight feeling in the chest area.
Such manifestations may accompany a person for several weeks, which should be considered an exacerbation of the disease.
What other symptoms are observed with HO? In addition to the main clinical picture, the following manifestations are possible in some cases:
- numbness of the upper extremities, a feeling of "goosebumps" passing through the skin;
- disturbance of the organs of the gastrointestinal tract;
- feeling cold in the legs, inability to warm up.
The hallmarks of such a disease are dorsago - a sharp pain between the shoulder blades and dorsalgia - a slow pain syndrome with no distinct image.
It should be noted that like any other type of osteochondrosis, chest disease often affects people who lead an inactive lifestyle. Continuous sitting in front of a computer, bending down, and strenuous physical exertion also become a provocative factor in the development of the disease.
How the disease manifests itself in women and men
The development of degenerative-dystrophic processes in the thoracic region of patients is considered a diagnosis - thoracic osteochondrosis. With this disease, the intervertebral discs are destroyed and there is malnutrition in the connective tissue structure. In addition, the circulatory process is interrupted because the chest area is inactive. And the pain syndrome itself occurs due to pinching of nerve endings during the progression of the pathology.
According to statistics, HO is sometimes diagnosed more often in women than in men, but at a younger age. The main reason for this phenomenon is the change in hormonal levels during the menopausal stage. Osteoporosis, which is often seen in women at the beginning of menopause, is also a factor in the development of the disease.
Therapeutic interventions are developed taking into account the clinical picture of the pathology. Severe symptoms do not appear immediately, and the disease is often suspected for a long time. In particular, it is already possible to make a diagnosis during a marked picture when the symptoms have become apparent. If it is an explicit period, two types of symptoms should be distinguished here:
- Development of painful feelings. . . Here in the chest region, we are talking about the occurrence of pain between the shoulder blades that radiates to the area of the solar plexus. Pain syndrome can migrate to the neck area, mimicking neck osteochondrosis and the arm. Often, women experience pain in the mammary glands, confusing them with breast pathologies. Feelings of pain are usually not permanent, they hurt, but they have no intensity.
- Blood pressure disorder. . . Women with osteochondrosis of the breast have a hypertensive syndrome characterized by increased pressure and can trigger a hypertensive crisis. A distinctive feature of normal hypertension may be the presence of minimal effect of antihypertensive drugs. In case of similar situations, you should consult a vertebrologist.
In addition to the above, other signs of degenerative-dystrophic disorders of the thoracic spine should be distinguished:
- Pain in the left side of the chest regiondoes not cause heart damage. . . In medical terminology, this phenomenon is called cardialgia. It is not difficult to diagnose, as the development of such a symptom cannot be stopped with the use of heart medications.
- Disruption of the digestive system. . . Often, with the onset of progression of osteochondrosis, problems begin with the internal organs, more often the gastrointestinal tract. The most striking examples are the development of heartburn, an increase in acidity and a feeling of constant bloating. Among other things, there may be problems digesting food - nausea after a meal, heaviness, bloating. Against the background of the above, the work of the chair is also interrupted - frequent constipation or diarrhea.
- Respiratory disorders. . . Because the dystrophic process occurs in the chest area, cases of respiratory violation are not uncommon. This is accompanied by unjustified dizziness, general weakness, shortness of breath and other signs that are indirectly similar to heart pathology or pressure problems (arterial / intracranial).
As for therapy, it largely depends on the signs of the pathological process. Painkillers, including NSAIDs in the form of ointments or gels, are prescribed to relieve pain. During the exacerbation period, muscle relaxants are more effective, reduce smooth muscle spasms, relax muscles, relieve pain syndrome, and have positive reviews of their use. When the pain becomes completely unbearable, a blockade is used with painkillers.
Chest treatment
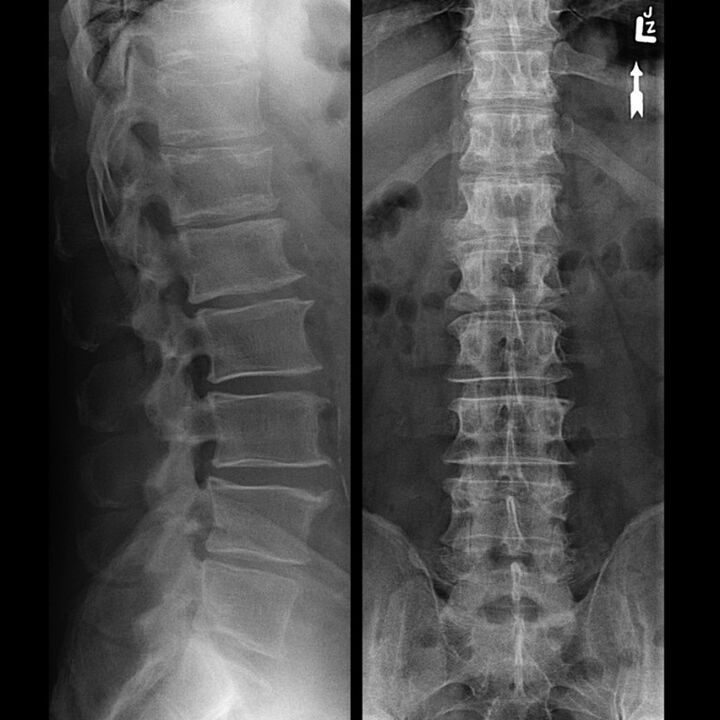
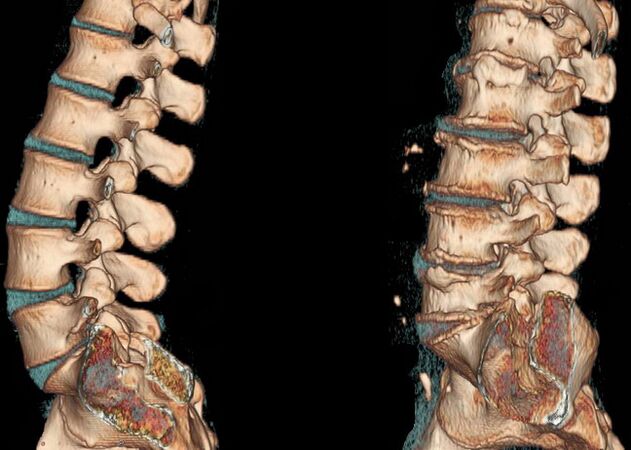
Exactly how your GO will manifest itself depends on the abnormalities that take place in the intervertebral discs. There are four stages in the course of degenerative-dystrophic disorders of the chest:
- The first. . . The symptoms are not particularly pronounced, but the process of drying out the plates of the thoracic spine has already begun. As a result, they lose their flexibility, get a flatter look, and still withstand certain loads. Occasionally, painful painful feelings are disturbed but not mild and often do not require painkillers.
- The second. . . At this stage, negative changes affected the annulus fibrosis, various types of damage can be observed - cracks, loss of stability. There are changes in the pain syndrome, it becomes more intrusive, palpable, increases with increasing motor activity - in bends and turns.
- The third. . . The rupture of the annulus fibrosus is clearly visible on the X-rays, and hernia begins to form. Feelings of pain become clearer, sharper from a whining character, intensified with movement and calm.
- Fourth. . . Spondyloarthrosis is actively developing in the background of vertebral convergence and disc erasure. As a result, the connective tissue of the annulus fibrosus is replaced by bone tissue, which significantly limits motor ability.
The clinical picture of osteochondrosis of the chest is such that this disorder is more likely to be diagnosed:
- Pain. . . Its localization is almost always in a specific location, often on the left. After a while, it spreads all over your chest, making it difficult to breathe, making it difficult to climb stairs or workout.
- Increased pain. . . Strengthening occurs when turning or tilting, usually with any physical activity, and the same can be observed when trying to take a deep breath.
- Muscle cramp. . . The above symptoms are accompanied by muscle cramps, with the contraction occurring mostly in the upper back. In rare cases, this symptom occurs in the lumbar region.
Special mention should be made of intercostal neuralgia, which lasts for several weeks and then disappears on its own. During this time, the person is accompanied by chest discomfort aggravated by movements, an uncomfortable feeling when trying to take a deep breath and exhale. Women may have the impression that they have problems with their mammary glands, which makes them think about their treatment, and men may feel a foreign object behind the sternum.
It should also be noted that the overall clinical picture described above is enhanced after night or hypothermia. The next morning it usually gets easier, but in the evening everything repeats itself.
How to treat, what methods exist, what to take? As for therapeutic measures, they should be started as early as possible. It can often be done in the very first stages even without the use of medication, but only with regular gymnastics - gym therapy.
The later stages of the development of the pathology, in 2 degrees, involve the use of drugs. This includes the different groups of drugs, the most popular are shown in the table below.
| Group of drugs | The main effect of the drug |
|---|---|
| Analgesics, analgesics | They alleviate pain syndrome, reduce its manifestation. |
| Non-steroidal anti-inflammatory drug (NSAID) | Eliminates inflammation, relieves pain and swelling. |
| Chondroprotectors | It increases the production of intra-articular secretions, slows down the process of cartilage destruction, reduces the manifestation of the inflammatory process. |
| Muscle relaxants | They reduce the tone of the skeletal muscles, they have a relaxing effect, they help to cope effectively with back pain. |
| Sedatives, sedatives | For more effective therapy, as severe pain can cause stress, which worsens the effect of treatment. |
In addition to essential medications, a drug-vitamin regimen is recommended.
In the event that the overall clinical picture worsens, the main goal of therapy will be to relieve symptoms. For a more pronounced and faster effect, painkillers are prescribed in the form of injections as well as steroid-type.
After cessation of exacerbation and achievement of stability, basic therapy should be initiated. A fairly wide range of drugs can be prescribed, as only a complex effect on the disease can yield positive results.
The main drugs are described in the table above and then in more detail about them. So basic treatment involves prescribing such drugs:
- Chondroprotectors.It is used in the form of tablets and for topical therapy, in the form of ointments or gels. It is impossible to rule out the use of such drugs, they form the basis of the entire therapy. Their effect is to inhibit cartilage tissue destruction and further progression of dystrophic changes. They also increase the ability of cartilage to regenerate. However, with the help of such a drug, it is impossible to get rid of the pathology completely, it should not be considered a panacea.
- Vasodilator. . . These are needed to improve blood circulation and, accordingly, nutrition in the affected area. Most often, a fairly effective medication is prescribed that improves blood microcirculation, helping to cope with pain at rest.
- Local therapy. . . Ointments or gels are prescribed for best effect. Thus, good results can only be achieved with a complex effect, so it is common to further recommend ointments from the same pharmacological groups when prescribing NSAIDs and chondroprotectors. Also popular are bee or snake venom-based creams that have a pronounced analgesic effect and are a good complement to the main therapy.
- Vitamins. . . In particular, group B vitamins are prescribed, which have analgesic properties to help cope with inflammatory processes and damage to nerve endings.
- Without error, a physiotherapy course, therapeutic massage, and hands-on therapy are prescribed along with the drug effect.
What other therapies should be incorporated into the treatment of chest osteochondrosis? An experienced professional strongly recommends the following techniques:
- magnetotherapy, electrophoresis, medicinal mud;
- complex of physiotherapy practices;
- acupuncture, acupressure.
In addition, it is recommended to follow a certain diet, you should exclude the consumption of alcohol, spicy foods, reduce the use of salt.
Particular attention should be paid to therapeutic exercises, performed daily, preferably several times a day. Please note that the exercises are developed individually by your doctor - orthopedist or traumatologist. Physical education is performed in the absence of exacerbation, when there is no pronounced pain, in the case of acute pain syndrome, maximum rest should be observed.
The sport of osteochondrosis is not the last thing. With this pathology, it is important to perform all the prescribed exercises on a regular basis that will strengthen the muscles and positively affect the outcome of the treatment.
We must also mention traditional medicine. There are many recipes based on natural ingredients on the Internet. It is not recommended to delight yourself with folk remedies as a stand-alone method, as their effectiveness will be minimal, in many cases zero. However, as a supplement to mainstream therapy, folk remedies have been suggested. The following homemade recipes are known:
- Ingredients for the first: 3 tablespoons rye flour, 1 tablespoon turpentine and a teaspoon iodine and garlic. We mix everything thoroughly and use it as an ointment at night.
- For the second: 5 tablets of metamizole sodium and 5 ml of camphor alcohol. Leave the tablets to a powder, then pour in alcohol and use overnight.
The needle applicator is another alternative therapy. Its effect is to reduce pain syndrome with the help of needle massage.

In the event that each of the described therapeutic methods has not produced the desired result or has been found to be non-permanent, the question of prescribing surgery will be decided. Surgical intervention is required if elimination of pain syndrome is not possible, the degenerative-dystrophic process continues to develop, however, negative changes in the functioning of internal organs can be observed. If your doctor continues to advise you to have surgery, you should not refuse immediately. Timely intervention allows you to get rid of such a problem, completely restore the work of the organs, and preclude the further development of complications.
Surgery usually consists of two stages. The first is to eliminate the cause - decompression - as a result of which the pain syndrome disappears. The second stage is the subsequent stabilization of the spine.
Osteochondrosis of the thoracic region is a serious pathology that can not only disrupt the functioning of the musculoskeletal system but also negatively affect the systems and organs.
It is important to monitor your own health, take preventative measures, monitor your diet, and pay attention to physical activity. Regular exercise is an effective prevention of osteochondrosis, but keep in mind that any load should be moderate.
Treatment of the cervicothoracal type
Osteochondrosis of the cervicothoracic region is not considered an independent pathology. In this case, we are talking about a set of abnormalities that appear in the intervertebral discs and are able to affect muscle tissue as well as nearby organs.
Cervicothoracic osteochondrosis is by no means uncommon, with more than 20% of diagnoses attributable to the disease. The disease is very insidious, and the variability in the clinical picture is in many cases a suspicion of other non-spinal diseases in the physician. For example, your doctor may recommend the presence of angina pectoris, recommend taking a medication that ultimately simply does not work, and at worst, negatively affects the condition of your heart system. For this reason, it is very important to distinguish osteochondrosis from pathologies of the internal organs. Thus, dystrophic disorders of the cervicothoracic region are characterized by the following signs:
- common headache;
- loss of strength followed by dizziness;
- aching pains in the neck, shoulders, shoulder blades, a condition of muscle stiffness;
- compression of the intercostal nerve roots, resulting in pain syndrome, and its exacerbation;
- violation of blood pressure, from hypertension to hypotension may decrease, more often in women;
- decreased visual acuity, hearing aid problems (hearing loss);
- in men, a decrease in potency with nerve overload in the background of the disease.
An important point is to formulate the correct diagnosis, here a number of diagnostic measures will be required, which include: X-ray, ultrasound, MRI, CT.
Comprehensive treatment is mandatory and should include:
- medicines;
- various physiotherapy techniques;
- physiotherapy;
- non-traditional therapy (acupressure, acupuncture).
It is also important to pay attention to non-medicated measures, such as reducing physical activity, which includes minimizing strain, replacing the mattress, and purchasing an orthopedic pillow.
Atypical symptoms, sensations and pain
In addition to the typical pains in thoracic osteochondrosis, there are a number of atypical pains that cannot be associated with spinal diseases. However, you should be aware of them:
- Heartache. . . It is common for such pathology to cause heart pain while mimicking the attacks of a heart attack. One of the distinguishing features is their duration. Unlike true heart pain, osteochondrosis can be painful for several weeks. In addition, the use of conventional medications does not reduce the onset of pain. Here it is worth thinking about the presence of a pathology other than the heart.
- Imitationpathologies of the mammary glands. . . This clinical picture is directly relevant to patients. Chest osteochondrosis often makes a person think about breast disease because a woman can observe pain in the chest region that spreads to the glands for a long time. It is only possible to identify the true cause of such a symptom, or at least rule out problems with the mammary glands, after an examination by a mammologist.
- Pain in the abdominal cavity. . . This symptom suspects the presence of gastritis and other gastrointestinal disorders. A gastroenterologist may mistakenly diagnose pancreatitis or cholecystitis. Such diagnoses can be refuted or confirmed by thorough investigation.
- In addition to these signs, the patient may experience severe painchest discomfortdescribed as a foreign object. It is often difficult to take a deep breath or exhale, the feeling that it is impossible to breathe deeply with shortness of breath with little physical activity.
The process of treating degenerative-dystrophic diseases is not easy, it requires a long time, effort of the patient and training of the treating physician.
Be sure to consult your doctor before treating any illness. This helps to take into account individual tolerance, confirm the diagnosis, ensure that treatment is correct, and rule out negative drug interactions. If you use a prescription without consulting your doctor, you do so entirely at your own risk. All information is for informational purposes only and does not constitute a medical aid. You are solely responsible for the application.

























